THE ROLE OF EPIDURAL INJECTIONS IN MANAGING YOUR SPINAL PAIN
What Do Epidural Injections Treat?
Epidural injections are a reliable treatment for helping manage spinal pain. Depending on your pain’s location, you could receive an injection in your cervical (neck) area, thoracic (upper to mid-back) area, lumbar (lower back) area or caudal (tailbone) area. These injections are helpful in relieving pain caused by problems with your discs, the parts of your spine that act like shock absorbers and separate your spinal bones, called vertebrae, from each other. Common causes of disc-related pain include disc herniation, or a bulging of the disc against a nerve, and what is called discogenic pain, pain that is caused by something wrong with the disc. For example, these discs can tear. If that happens, part of the disc will start to leak chemicals. This can cause inflammation to the nerve roots resulting in pain. Epidural injections are also used for recurrent pain after surgery and for spinal stenosis.
The type of epidural injection you receive will depend on where the pain is located and what is causing your pain. It’s important to know that pain in one area of your body often has its source in a totally different area. For example, a problem in your neck can cause pain in your head, your shoulder blades, or somewhere in-between, on either the left or right. A problem in your upper back can cause pain in your shoulders, upper back, lower back, or hips, on either the left or right. A problem in your lower back can cause pain in your lower back or your buttocks, on either the left or right. Epidural injections can also be classified as caudal, interlaminar, and transforaminal. The laminae are part of the structure of each vertebra, so an interlaminar injection is one that is performed between the laminae. The foramen is an opening in the vertebra that a nerve root passes through, so a transforaminal injection is one that goes across this opening. A caudal injection is given into a small opening above your tail bone, called the sacral hiatus
Injections are used for treating pain caused by:
1. Disc Herniation
2. Radiculitis or Radiculopathy
(pain related to nerve roots)
3. Spinal Stenosis, or narrowing of the spinal canal
4. Postsurgery Syndrome
5. Discogenic conditions
6. Complex Regional Pain Syndrome
7. Postherpetic Neuralgia (a complication of shingles)
8. Chemotherapy-related or Diabetic Neuropathy.
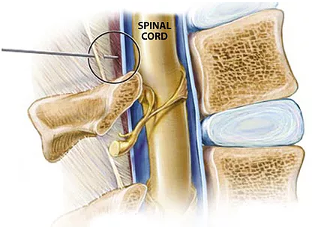
Your spinal cord, and the nerves connected to it, are protected by a covering in the form of a sac, called the dura. The dura contains the spinal fluid. The region surrounding the dura is called the epidural space. A leaking disc as described earlier can also cause irritation and pain to the dura.
If your injection’s purpose is to help  your doctor diagnose where your pain originates, then a local anesthetic will be used. If it is to treat your pain, then an anesthetic with or without steroid will be used. The anesthetic is to help numb the cause of your pain and help inflammation and the steroid is for treating the inflammation.
your doctor diagnose where your pain originates, then a local anesthetic will be used. If it is to treat your pain, then an anesthetic with or without steroid will be used. The anesthetic is to help numb the cause of your pain and help inflammation and the steroid is for treating the inflammation.
Based upon your individual situation, your doctor or your doctor’s medical staff will give you specific instructions on how to prepare for your procedure. In general, you may eat a light meal within a few hours before the procedure. If you are an insulin dependent diabetic, do not change your usual eating pattern before the procedure. If you are taking medications, you will be given instructions on whether or not to take them. Also, if you are taking a blood thinner, such as Coumadin®(warfarin sodium), you should tell your doctor. Many over-the-counter medicines such as aspirin and ibuprofen also thin the blood. Stroke prevention medications, such as Plavix® (clopidogrel bisulfate), affect blood thinness and clotting. Be sure to let your doctor know the name of every single medication you take. You might be instructed to temporarily stop using these medications for as much as a week prior to your procedure.
To help you relax, you will be given Intravenous therapy. A local anesthetic will be applied to your skin. Depending on the particular injection you will receive, you could be seated, lying on your side, or lying face down. Using a thin needle, the doctor will inject you right in the epidural space. The doctor might even inject a dye, or use a special type of x-ray called fluoroscopy to help guide the needle’s positioning. When your doctor is sure the needle is in the right place, the anesthetic with or without steroid will be injected.
After your injection, medical staff will monitor you for  approximately a half-hour. Some patients will feel immediate pain relief. It is normal to feel numbness in the treated area immediately following your procedure. This can last up to six hours. You may even want to move the area in the same way that used to cause pain, just to see how well your injection is working. Please, do not move the area too much or too quickly!
approximately a half-hour. Some patients will feel immediate pain relief. It is normal to feel numbness in the treated area immediately following your procedure. This can last up to six hours. You may even want to move the area in the same way that used to cause pain, just to see how well your injection is working. Please, do not move the area too much or too quickly!
It is also normal for your pain to come back briefly after going away. The return of your pain could last for up to two days and might even be somewhat worse than it was before. If your injection contained a steroid, then that steroid might be causing this new discomfort; another possibility is irritation caused by the injection needle. The steroid usually will take about two or three days before being effective. In some cases it can take a week. You might be given a pain journal to track how your pain goes away in the days after your procedure. Returning to work or other daily physical activities depends on your individual situation. Your doctor will discuss this with you. Some patients receive long-term pain relief from just one injection. For others, the relief might only last a few weeks and further treatments will be needed. Generally relief occurs in approximately 13-16 weeks with one injection. Relief is only weeks initially and stabilizes after two injections. Pain caused by additional irritations will have to be treated separately.
After your recovery on-site, you will be released to go home.  Someone will need to drive you, since you should not drive or operate machinery for 12 hours after treatment. Also, you should not make important decisions from 12-24 hours. You might require some assistance in walking or getting around. Basically, just rest and take it easy. You can take your usual medication when you get home and even resume your regular diet. If your injection site hurts, ice or heat can be applied. If your IV site hurts, place a warm towel on it for twenty minutes, two-to-three times a day. Most patients tolerate this procedure quite well. However, if there is a major change in your pain pattern or the amount of your pain, if you have excessive or abnormal bleeding, or if you experience persistent chills or a fever over 100 degrees Fahrenheit, call your doctor’s office right away. If you cannot reach the office, go to the nearest hospital emergency room.
Someone will need to drive you, since you should not drive or operate machinery for 12 hours after treatment. Also, you should not make important decisions from 12-24 hours. You might require some assistance in walking or getting around. Basically, just rest and take it easy. You can take your usual medication when you get home and even resume your regular diet. If your injection site hurts, ice or heat can be applied. If your IV site hurts, place a warm towel on it for twenty minutes, two-to-three times a day. Most patients tolerate this procedure quite well. However, if there is a major change in your pain pattern or the amount of your pain, if you have excessive or abnormal bleeding, or if you experience persistent chills or a fever over 100 degrees Fahrenheit, call your doctor’s office right away. If you cannot reach the office, go to the nearest hospital emergency room.
Complications
Spinal injection procedures are generally safe procedures. If complications occur, they are usually mild and self-limited.
The risks of spinal injections include, but are not limited to:
Bleeding
Infection
Nerve injury
Thinning of the bone
Paralysis
Avascular necrosis
Spinal headache
Muscle weakness
Increased pain
Common side effects from steroids include:
Facial flushing
Increased appetite
Menstrual irregularities
Nausea
Diarrhea
Increased blood sugar
Arthralgias
Some people are not good candidates for spinal injections. These include people with:
Active systemic infection
Skin infection at the site of needle puncture
Bleeding disorder or anticoagulation
Uncontrolled high blood pressure or diabetes
Unstable angina or congestive heart failure
Allergy to contrast, anesthetics, or steroids